A Guide to the No-Scalpel Procedure: Open Ended Vasectomy
An open-ended vasectomy offers a modern solution for permanent contraception with fewer complications and less discomfort. Unlike traditional methods, it leaves one end of the vas deferens open, which helps in reducing post-operative pain. This guide will explore how the procedure works, its benefits, and why many men choose this method of vasectomy.
What is a No Scalpel, Open-Ended Vasectomy?
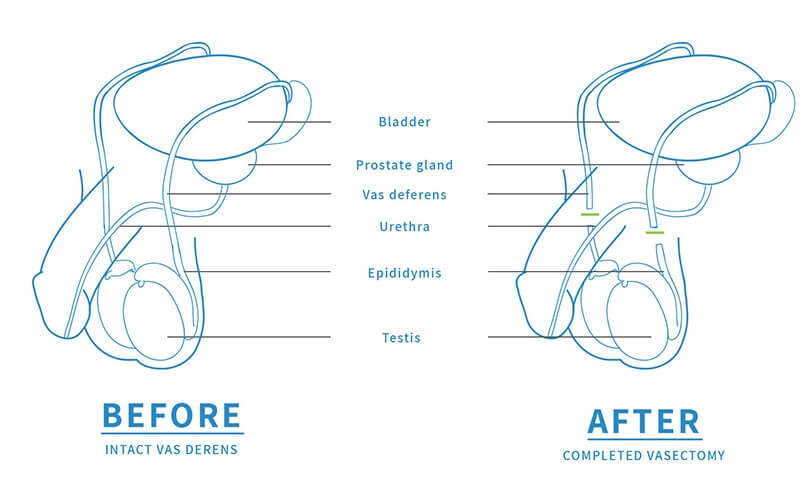
A no scalpel, open-ended vasectomy is a surgical procedure designed to provide effective permanent contraception while minimising potential discomfort and complications. Unlike traditional methods, this technique involves leaving one end of the vas deferens open, allowing sperm to exit the testes but preventing it from mixing with semen.
This method facilitates the natural reabsorption of sperm by the body, which helps to minimise pressure and discomfort. Open-ended vasectomy provides a modern solution to male vasectomy, ensuring effectiveness and comfort.
How Does an Open-Ended Vasectomy Differ from a Traditional Vasectomy?
Several key differences distinguish an open-ended vasectomy from a traditional one. Notably, the procedure time for an open-ended vasectomy is generally shorter, usually around 15 minutes, compared to the 30 minutes or more required for traditional methods. This shorter duration enhances convenience and reduces patient stress and anxiety.
The recovery process also sets open-ended vasectomies apart. Being less invasive, they lead to quicker and easier recovery times, with patients typically experiencing less post-operative pain and discomfort, enabling a faster return to normal activities.
Additionally, the open-ended technique significantly lowers the risk of post-vasectomy pain syndrome.
The No-Scalpel Approach in Open-Ended Vasectomy
The no-scalpel vasectomy technique involves accessing the vas deferens through a small incision in the skin, typically between 5mm - 8mm in size.
One of the primary benefits of the no-scalpel technique is the reduced risk of complications such as infection and bleeding. The absence of stitches and minimal size of the incision contribute to quicker recovery and less discomfort.
By maintaining the testicular end of the vas deferens open, this method allows for the natural absorption of sperm, reducing the risk of inflammation.
Overall, the no-scalpel approach represents a significant advancement in vasectomy techniques, offering a safer and more comfortable option for permanent contraception.
Procedure Steps for an Open-Ended Vasectomy
Preparing for an open-ended vasectomy involves several crucial steps. Patients should attend a pre-procedure consultation to understand the process and how to prepare, which may include stopping certain medications and arranging time off work. This preparation ensures that patients are fully informed and ready.
- A local anaesthetic is injected into the area using a fine needle. A tiny hole 5mm-8mm long is made in the scrotum.
- The vas deferens is divided and the testicular end of the tube is left open to help prevent congestion in the testis. A tiny layer of tissue is placed between the two ends of the vas to stop them re-joining.
- The same procedure is performed on the other side but through the same hole. The skin edge is clipped together without stitches.
- Sex and physical activities can be resumed within a few days. Back-up contraception is essential until the follow-up test 3 months after the vasectomy procedure. Read more here: How soon after vasectomy can you have sex.
The entire procedure typically takes about 20 to 30 minutes, making it a relatively quick and efficient option for permanent contraception. With proper preparation and skilled execution, the open-ended vasectomy provides a straightforward and effective solution for long-term birth control.
Possible Risks and Complications
Like any surgical procedure, an open-ended vasectomy procedure carries certain risks and potential complications. Risks to be aware of include:
- Bleeding and infection after the vasectomy. Rest and support reduces this risk.
- Forgetting to use contraception during the first three months after the vasectomy procedure, resulting in early pregnancy.
- A natural re-joining of the tubes, which can occur even if the procedure goes perfectly on the day
- A small number of men (1-2%) may develop longer term pain beyond 3 months.
The no-scalpel vasectomy procedure, in particular, involves very little discomfort during the procedure and lowers the likelihood of complications like post-vasectomy pain syndrome.
Importantly, no life-threatening complications are associated with no-scalpel vasectomies, making it a reliable and safe choice for permanent contraception. Understanding these potential risks and benefits helps patients make informed decisions about their vasectomy options.

Recovery and Aftercare
Recovery from an open-ended vasectomy is generally smooth, thanks to the minimal post-operative complications associated with the procedure. Patients often experience less bruising and swelling due to the no-scalpel method, which contributes to a more comfortable recovery.
To aid vasectomy recovery, applying ice packs or a pack of frozen peas to the scrotum for 20 minutes each hour can minimise swelling. Resting with elevated feet during the first few days also helps reduce swelling in the testicles. Wearing supportive underwear, provides additional support and comfort during the recovery period. Read vasectomy recovery tips for Melbourne men here.
Avoiding swimming or baths for the first 2-3 days post-surgery helps prevent infection. Refraining from strenuous activities, including sports and heavy lifting, for at least two weeks is also recommended. Following these guidelines ensures a smooth recovery and reduces the risk of complications.
Lastly, using contraception for a few months after the vasectomy is essential to avoid unintended pregnancy. Patients are generally advised to use contraception for three months following the procedure, as it takes time for any remaining sperm to be cleared from the system. Adhering to these aftercare instructions ensures the best possible outcomes from the vasectomy.

Success Rates and Effectiveness
Open-ended vasectomy is recognised as a highly effective option for permanent contraception, with an effectiveness rate exceeding 99%. This high success rate makes it one of the most efficient forms of birth control.
Reversibility of Open-Ended Vasectomy
While vasectomy reversals are possible, it's best to have the mindset that the vasectomy procedure is permanent. Vasectomy reversal is expensive and usually not covered by health insurance. However, open-ended vasectomy reversals are generally easier and more successful than reversing a traditional closed-ended vasectomy. Success rates for reversal can range from 30% to 95%, depending on various factors.
Other factors that influence the success of a reversal include the female partner’s age and whether the same partner is involved, as prior fertility with the partner suggests a higher chance of successful conception. By considering these factors, patients can make informed decisions about the potential for vasectomy reversal.
Choosing the Right Vasectomy Doctor
Choosing the right vasectomy doctor is crucial. Verify that the doctor holds additional training in the Li No-Scalpel Vasectomy technique. Consultations are essential for discussing concerns and preferences with the doctor before proceeding with vasectomy. Patients should understand the specific technique used as different methods can affect comfort and recovery. Choosing a qualified and experienced doctor ensures a smoother procedure and better outcomes.
Cost Considerations
Understanding the costs involved in an open-ended vasectomy is important when it comes to making an informed decision. A Medicare rebate applies to the procedure. Patients typically pay a booking fee and the remainder before the procedure, and can claim a portion from Medicare.
In summary, an open-ended vasectomy combined with the no-scalpel technique offers a highly effective and minimally invasive solution for permanent contraception. This method not only reduces the risk of post-operative complications but also enhances patient comfort and recovery. By leaving one end of the vas deferens open, the open-ended technique helps manage sperm more effectively, reducing the likelihood of post-vasectomy pain syndrome and other issues.
Choosing the right vasectomy doctor and being well-informed about the procedure, costs, and potential risks are crucial steps in making a decision. Whether you are considering this procedure for its high success rates, lower discomfort, or ease of reversibility, a no scalpel vasectomy represents an efficient and reliable option for long-term birth control.