A vasectomy is a quick and effective procedure for long-term birth control. It typically takes just 15–30 minutes in the clinic, a couple days of rest, and back to normal in no time.
However, certain medical conditions can make the procedure a bit more difficult or affect how you recover. That doesn’t mean you can’t get a vasectomy, it just means your doctor may need to adjust the approach, take extra precautions, or help you plan for a longer recovery.

If you have any of the following conditions, it’s important to talk with your provider before the procedure.
Blood Disorders or Use of Blood Thinners
If you have a bleeding disorder such as hemophilia or you’re on blood-thinning medications like warfarin, aspirin, or newer anticoagulants, your procedure will require special consideration.
Vasectomy involves small blood vessels in the scrotum. If your blood doesn’t clot properly, you may have a higher risk of excessive bruising, swelling, or internal bleeding.
What your provider may do:
- Coordinate with your primary doctor or haematologist.
- Possibly adjust your medication schedule before the procedure with your specialists consent.
- Use extra care to control bleeding during the vasectomy.
Important: Never stop taking blood thinners without medical advice.
Epididymitis or History of Scrotal Infections
The epididymis is a coiled tube behind each testicle that stores and carries sperm. If you’ve had epididymitis inflammation or infection of the epididymis you might still be a candidate for vasectomy, but your provider will want to understand your history.
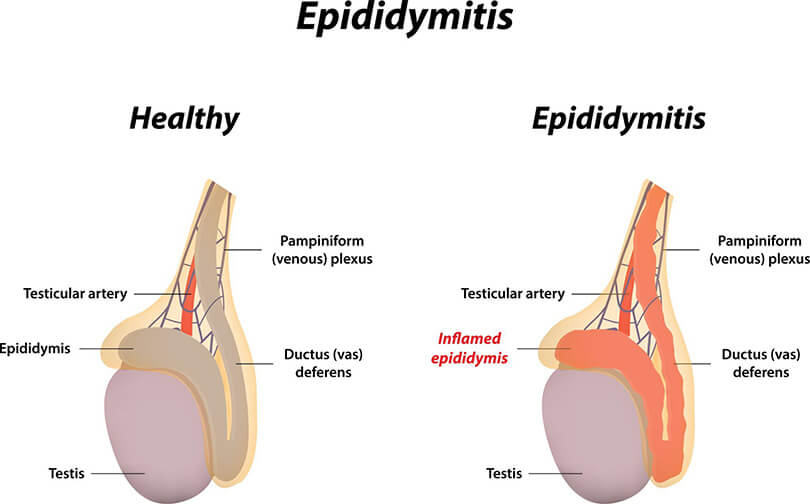
Ongoing or past inflammation can make the tissues more sensitive. There may be scarring, which could complicate the procedure, and it can also increase the risk of post-vasectomy discomfort or swelling.
What Dr Wilson may do:
- Review your medical records and ask about any past infections or pain.
- Recommend waiting until any infection or inflammation is fully resolved.
- Use a modified technique if needed.
Testicular Disease or Abnormalities
If you’ve had a testicular mass, cyst, or other testicular disease, it’s crucial to bring that up during your pre-vasectomy consultation. Some testicular conditions may not directly affect your eligibility for a vasectomy, but they could make the anatomy more challenging.
What Dr Wilson may do:
Conduct an exam and may recommend an ultrasound to check for any issues.
Delay the vasectomy until your other healthcare providers give the okay to go ahead.
Chronic Testicle Pain
If you regularly experience pain in your testicles especially if the cause isn’t known, let Dr Wilson know before booking your vasectomy. Chronic scrotal pain can sometimes become worse after the procedure, especially if the pain is nerve-related or not fully diagnosed It may also increase your risk of post-vasectomy pain syndrome (though this remains rare overall).
What your provider may do:
- Conduct a thorough exam to determine the cause of the pain.
- In some cases, recommend postponing the procedure or exploring other options.
Previous Scrotal or Inguinal Surgery
If you’ve had surgery in the scrotal area such as for a hydrocele, varicocele, hernia, or undescended testicle, your vasectomy may still be doable, but the path to the vas deferens could be different. Scar tissue from previous surgery can make it harder to access or isolate the vas deferens and there may be changes in anatomy or sensitivity in the area.
What your provider may do:
- Review your surgical history.
- Adjust the technique if needed.
- In some cases, refer you to a urologist for a more complex procedure.
Difficulty Isolating the Vas Deferens
Sometimes, even without any prior health conditions, the vas deferens, the tubes that carry sperm can be naturally difficult to locate or isolate due to body type, scarring, or previous trauma. Accessing the vas deferens is the key step of the procedure. If they’re hard to find or buried deep, the no-scalpel technique might need modification.
What your provider may do:
- Use extra tools or reposition you during the procedure.
- In rare cases, recommend referral for a more advanced surgical setting.
The Bottom Line

Having a medical condition doesn’t automatically disqualify you from getting a vasectomy. But it may mean we’ll need to plan a little more carefully to ensure your safety and comfort.
At Direct Access Vasectomy, we take the time to understand your health history and adjust the procedure to fit your needs. That includes working with other providers, reviewing medications, and keeping your risks as low as possible.
If you have any concerns about your eligibility for a vasectomy, we’re here to help. Schedule a consultation, and we’ll guide you through every step to help you understand the risks and put your mind at ease.